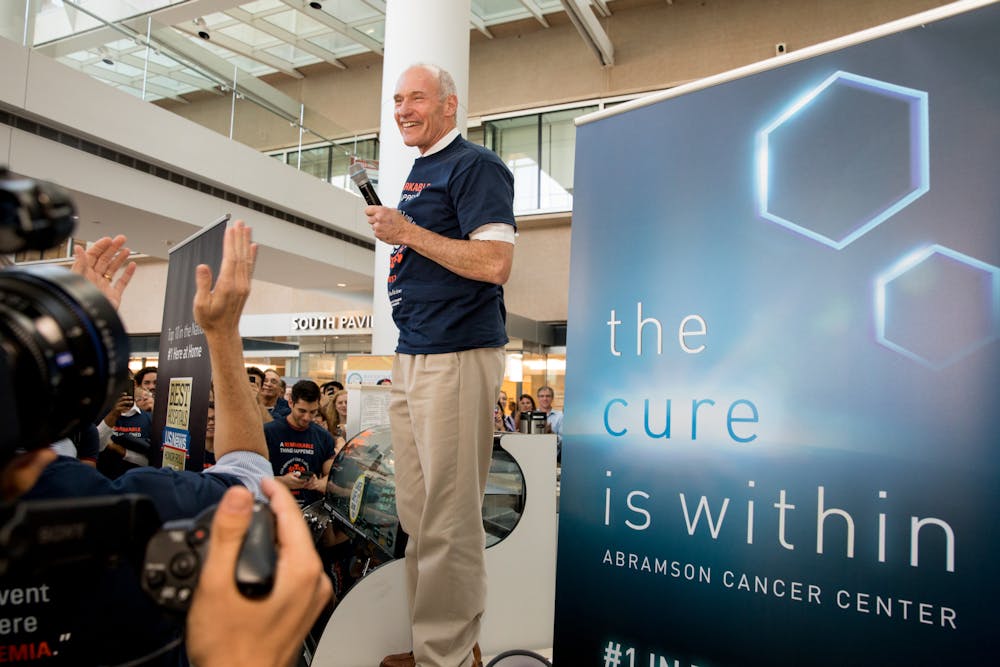
Perelman School of Medicine professor Carl June was named one of the winners of the 2024 Breakthrough Prize in Life Sciences.
June, the Richard W. Vague Professor in Immunotherapy in the Perelman School of Medicine and director of the Center for Cellular Immunotherapies at Penn Medicine’s Abramson Cancer Center, was awarded the prize for his work in creating and pioneering chimeric antigen receptor T cell immunotherapy, according to Penn Today. This treatment modifies a patient’s T-cells to target and kill their own cancer cells.
The Breakthrough Prizes were founded ten years ago by figures including Mark Zuckerberg and Sergey Brin, awarding $3 million for each of the five categories. June is the sixth Breakthrough Prize laureate from Penn, making Penn — along with Harvard and MIT — one of the most successful institutions in terms of receiving Breakthrough Prizes, according to Penn Today.
June joins Drew Weissman and Katalin Kariko, who won the 2022 Breakthrough Prize in Life Sciences for developing mRNA vaccine technology used in the Pfizer-BioNTech and Moderna COVID-19 vaccines. Other Penn faculty members who have won the Breakthrough Prize include Dr. Virginia M.Y. Lee (2019 - Life Sciences), Dr. Eugene Mele (2019 - Physics), and Dr. Charles Kane (2019 - Physics).
June previously won the Dan David Prize for his work on the first United States Food and Drug Administration-approved personalized cellular therapy for cancer treatment and the $1 million Sanford Lorraine Cross Award for his work in cancer cell therapy in 2021. June was also named one of Time Magazine’s 100 most influential people of 2018.
According to Penn Today, June’s lab engineered the gene-modified T cells for the first clinical trial for CAR-T cell therapy in 2010. Patients from this study were able to have decade-long leukemia remissions after they received CAR-C Tell treatments. In the decade since the first clinical trial, many CAR-T cell therapies have been approved for various subtypes of leukemia, lymphoma, and myeloma and autoimmune diseases such as lupus.
June and his team continue to push the envelope of how CAR-T therapies can treat blood cancers, solid tumors, and other diseases. Recently, they published an article in Science Translational Medicine about how CAR-T cells can target a protein on the surface of nearly all blood cancer cells named CD45. Using cell cultures and mouse models, the study showed that anti-CD45 CAR-T cells are able to eliminate acute myeloid leukemia cells in a very short time span of roughly three weeks.
Since CD45 is not only found in blood cancer cells but also in healthy blood cells, the researchers had to use a method called “epitope editing” to overcome the healthy blood cells. Epitope editing changes a small portion of the CD45 molecule by using CRISPR editing technology. The CAR-T cells then bind to this small piece of the CD45 molecule and attack it.
June, in a Penn Medicine press release, said that CAR-T cell therapy has the potential to drastically affect the way cancers are treated.
“One drawback of the current approach to CAR T cell therapy is that each therapy must be developed individually based on the targets for that cancer type,” June said. “This study lays the groundwork for a more universal approach that could potentially expand CAR T cell therapy to all blood cancers.”
The Daily Pennsylvanian is an independent, student-run newspaper. Please consider making a donation to support the coverage that shapes the University. Your generosity ensures a future of strong journalism at Penn.
Donate



