
The researchers in the Drew Weissman Laboratory, from left to right: Amir Yadegari, Tyler Papp, Hamideh Parhiz, Ousamah Soliman, István Tombácz, Xiomara Mercado-Lopez, Adam Sirusas, and Mohamad-Gabriel Alameh.
Credit: Sukhmani KaurOngoing research led by Penn professor Drew Weissman, whose breakthrough mRNA technology and therapy was a key part of the Pfizer-BioNTech and Moderna vaccine development for COVID-19, is continuing to pave way for innovative treatments for other global diseases.
Weissman said that his laboratory, located in the Hill Pavilion, is working on a wide variety of projects focusing on the larger potential of RNA, including its use in vaccines, gene editing, and mRNA therapeutics. These new projects come years after Weissman published research with Penn professor and BioNTech Senior Vice President Katalin Karikó in 2005 about the anti-inflammatory nature of RNA and its potential uses in vaccine delivery.
"[mRNA research] has enormous potential for vaccines, therapy, and gene therapy," Weissman told The Daily Pennsylvanian. "It can be applied to many diseases and will likely be found to be better than current approaches."
Researchers in Weissman's lab are currently working on three primary projects: developing new vaccines, replacing and editing proteins, and using mRNA to target specific genes.
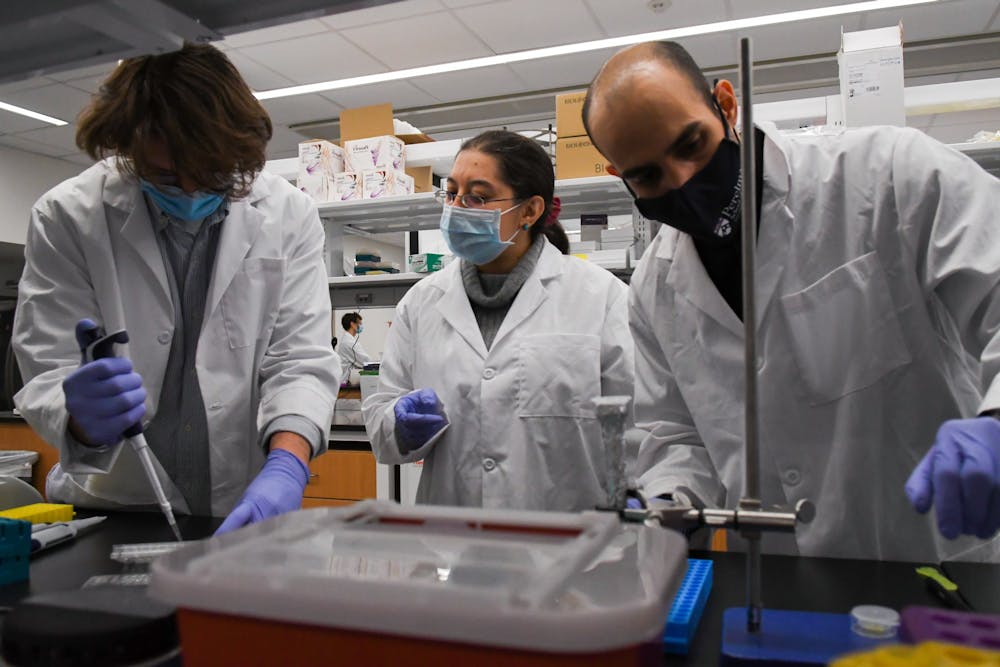
Weissman Lab researchers, from left to right: Tyler Papp, Hamideh Parhiz, and Amir Yadegari.
Using mRNA for COVID-19 vaccine developments
One of the main implementations of Weissman and Karikó's research has been in the area of studying and creating vaccines to solve unique problems, Mohamad-Gabriel Alameh, a researcher in Weissman’s lab, said.
“We are working on a new generation of vaccines — an improved generation,” Alameh said. “When you are talking about this improved generation, it means better vaccines that cover pan-coronavirus, which means all the potential coronavirus mutations or the other families of the virus like the seasonal coronavirus.”
According to the Centers for Disease Control and Prevention, there are currently five variants of concern within the United States. Many health experts, including Dr. Anthony Fauci, have asserted that a pan-coronavirus vaccine is necessary to protect against new variations that may arise.
István Tombácz, another researcher in Weissman’s lab, is working on developing such a vaccine. Without a vaccine that takes care of all possible strains, Tombácz said that “it is just a race against time” to develop new cures, as dangerous COVID-19 variants continue to emerge.
"There have been three coronavirus epidemics in the past 20 years," Weissman wrote in an emailed statement to the DP. "This means there will be more. We can either wait for the next one and shut down the world for a year, or develop a pan-coronavirus vaccine now and be prepared."
In addition to working on a pan-coronavirus vaccine, Weissman and researchers in his lab are working indirectly with the Thai government through Chulalongkorn University in Bangkok to help develop their own vaccine intended for people in Thailand and other surrounding nations, as the country is concerned about the availability of the Pfizer and Moderna vaccines in lower-income countries.
Weissman previously emphasized to the DP that while people in the United States, Europe, and other wealthy countries are getting the vaccine first, the pandemic will not be over until “the rest of the world” receives it too.
Alameh said that the Weissman lab has played a large role in developing a separate vaccine in Thailand. He said that the lab has been having regular meetings with Chulalongkorn University to review their data, and Alameh added that he helped produce 400 milligrams of RNA for their factory’s engineering trial. Weissman wrote to the DP that the Thai mRNA-based vaccine will be put it into clinical trials shortly.
While over 150 countries have begun vaccinating their populations, the "richer and more developed countries" have an advantage due to their existing health care infrastructure that can manufacture, acquire, and administer doses, according to data provided by Reuters. Approximately 59% of people who have received at least one dose of a COVID-19 vaccine are from high-income countries.

Researchers Mohamad-Gabriel Alameh and Ousamah Soliman discuss data in the Weissman laboratory.
Using mRNA to edit genes and replace proteins
Researchers in Weissman’s lab are also using CRISPR-Cas9 technology for gene editing in order to correct genetic diseases. This technology can either disrupt, delete, or insert segments of DNA in the genome by cutting the DNA precisely and allowing the natural repair process to take over.
Tombácz, whose work focuses on gene editing technology, said this work makes it possible to “knock in” the gene for a missing antibody to ensure the antibody will be produced permanently. This, Tombácz said, would be a possible way to treat individuals who are HIV-positive.
Since joining Weissman’s lab over three years ago, Tombácz said that seeing the potential effects of the lab's research has been rewarding and motivating.
“I just like science, and I like solving problems,” Tombácz said. “Of course, it's a plus if you know that the research is something useful, but when I actually do the experiment, it is not on my mind that this could help thousands of people.”
Using mRNA to target specific genes
Other researchers in Weissman's lab, like Hamideh Parhiz, are working on targeting genes for a variety of non-vaccine related applications. Parhiz, a research assistant professor of Medicine in the Division of Infectious Diseases, who has been working in Weissman’s lab since 2018, primarily focuses on treatments for acute inflammatory conditions where the mRNA only needs to be in a specific tissue or cell type.
While Parhiz said she has been interested in gene therapy for the past 10 to 15 years, she grew more interested in the potential of mRNA after joining Weissman’s lab. Looking to the future, Parhiz said that companies like Pfizer and Moderna showing interest in the potential of mRNA technology has made further research in the field more practical.
Both the Pfizer and Moderna vaccines are the first vaccines that use mRNA to be distributed at the current scale. According to data from the Centers for Disease Control and Prevention, over 160 million doses of the two vaccines have been administered across the United States thus far, and over 62 million Americans have been fully vaccinated by the Pfizer or Moderna vaccine.
“The production of the COVID-19 vaccine actually made research possibilities in mRNA fields much, much easier now to move forward,” Parhiz said. “Messenger RNA technology has definite potential, way beyond just vaccines, and that is how I see the future of this field going. In a few years, we will have different types of applications and different [areas of medicine] that will benefit from mRNA technology.”
The Daily Pennsylvanian is an independent, student-run newspaper. Please consider making a donation to support the coverage that shapes the University. Your generosity ensures a future of strong journalism at Penn.
Donate






